Bulimia Nervosa
Bulimia is a serious eating disorder characterised by binge (or excessive) eating, followed by methods used to prevent weight gain and discard the food eaten. The majority of patients suffering from bulimia choose to vomit or purge the excess food.
Bulimia Nervosa
Bulimia is life-threatening, causing both physical and psychological harm to the body. Over time, bulimia can negatively impact the body in several ways such as:
Stomach damage from over eating.
Electrolyte imbalance (having levels of sodium, potassium, or other minerals that are too high or too low, which can lead to heart attack or heart failure)
Throat pain and ulcers in the throat (due to a frequent flow of gastric acid that deteriorates oesophagus and stomach lining)
Anxiety, guilt or mood swings
Absence of menstruation or irregular menstruation
Bad breath, dental cavities, and dry mouth
Mucositis (when your mouth or gut is inflammed, commonly associated as a side effect of chemotherapy and radiotherapy)
In patients suffering from bulimia, the most notable impact is a very damaged and unhealthy set of teeth due to the gastric acid eating away minerals that form the tooth enamel.
Patients suffering from gastric reflux would display the same tooth erosion due to the continual backward flux of the hydrochloric acid within the stomach.
This can affect the appearance of your teeth and open the door for harmful bacteria which cause cavities.
Anorexia Nervosa
Anorexia is a serious eating disorder characterised by a person’s extreme desire to lose weight, causing them to become obsessed about what they eat.
Anorexia Nervosa
With an unwarranted fear of being overweight and a distorted body image, a patient suffering from anorexia can starve themselves or choose to over exercise. Likewise, they tend to follow certain restrictive diets consisting of very few food variety, which then negatively impact their body with effects such as:
nutrition deficiency
electrolyte imbalances
hair loss
brittle hair and nails
unhealthy, dry skin
constipation
lethargy, lack of energy, exhaustion
delay puberty and slow growth
depression, anxiety and/or guilt
tooth erosion and gum disease (due to lack of saliva production and/or following an extremely acidic diet can also escalate the symptom)
Chronic Gastroesophageal Reflux (GERD)
Gastroesophageal reflux disease (GERD) occurs when stomach acid repeatedly flows back into the tube connecting your mouth and stomach (oesophagus). This backwash (acid reflux) can irritate the lining of your oesophagus. The action of acid reflux can also be called acid regurgitation.
If you have acid reflux for more than two weeks, you are classified as having (GERD).
Some symptoms of GERD include:
nausea
chest pain
pain when swallowing
difficulty swallowing
chronic cough
a hoarse voice
bad breath
Progression of Gum Disease
Tooth Erosion Pattern
Erosion or wear is caused by the introduction of corrosive agents has a satiny finish . Erosion often occurs in areas where other tooth surfaces can't touch.
The distribution of lesions from dental erosion due to intrinsic acid regurgitation and vomiting may be different from patterns of dental erosion due to extrinsic acids. There are two types of erosion: intrinsic and extrinsic.
Intrinsic erosion usually comes from regurgitated stomach fluids, i.e, reflux or bulimia. Intrinsic erosion most commonly affects the lingual and occlusal surfaces of teeth and may be asymmetric as in the wear of GERD:
Intrinsic erosion
Extrinsic erosion is caused by ingested acidic substances and will show up on the facial and occlusal surfaces of teeth and is often worse in the lower arch.
Extrinsic erosion
Treatments To Restore Damaged Teeth From Erosion
Because damaged tooth enamel does not naturally regenerate, specialised treatment proposed by qualified dental practitioners is needed to repair your tooth.
Dental erosions can be treated with:
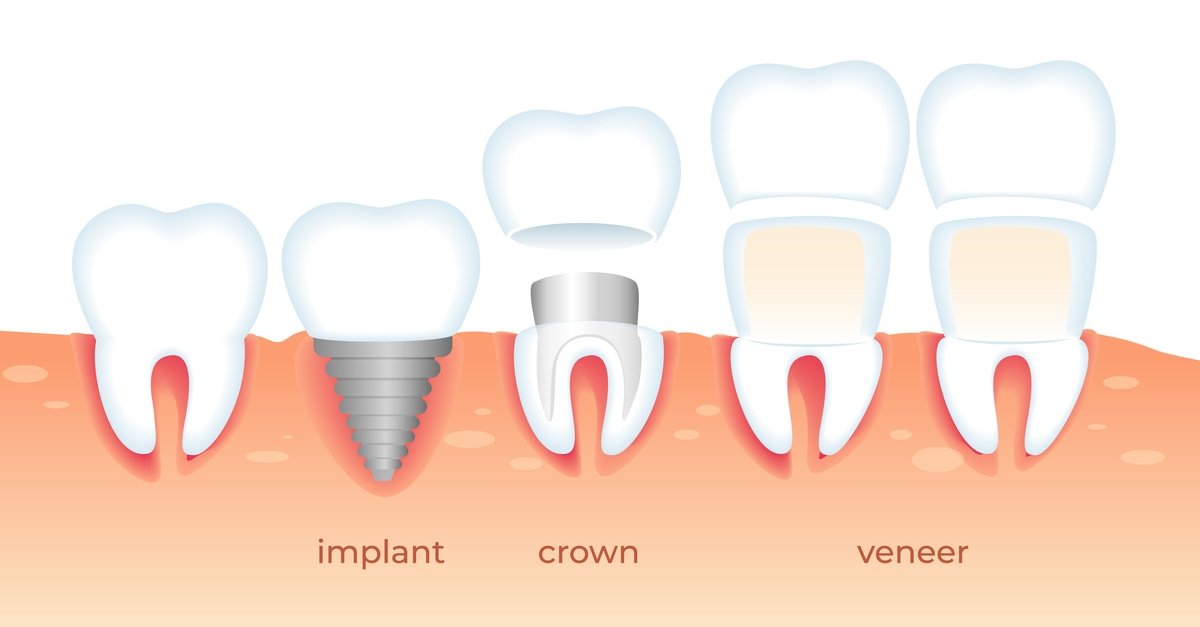
Dental veneers
Fillings
Crowns
Root canal treatment, or
Tooth extraction and/or tooth implant
As gastric acid erodes many teeth at once, crowns and fillings are the most popular treatments for restoring patients’ teeth.
Treatments To Restore Damaged Teeth From Erosion
Tooth erosion conditions vary from person to person. The best course of action is to contact a dental practice for a consultation so that the dentist is able to propose a treatment plan.
At Pain Free Dentist Sydney, we are proud to provide excellent dental service that is completely pain-free. Along with Dr. Lisa Chong’s 25 years of experience in general dentistry, dental implants, and specializing in TMJ dysfunction, you can certainly allow yours f to be under our care worry-free!
Please do not hesitate to give us a call at 9558 8988. Alternatively, you can try to reach us via email info@painfreedentistsydney.com.au if you have any health inquiries or problems.
What foods cause tooth erosion?
Tooth erosion is different from tooth decay because erosion is not caused by bacteria, but rather by the wearing down of the tooth enamel due to eating acidic food. Common foods which cause tooth erosion are acidic. Your enamel is mostly made of crystals of a mineral called hydroxyapatite. This mineral structure can start to dissolve if surrounded by acids of pH lower than 5.5, creating holes in the teeth called cavities. Some foods which cause tooth erosion can include:
Citrus fruits or fruit juices, especially lemon, orange, cranberry or apple juice.
Soft drinks (containing phosphoric and citric acid).
Sugar (is not acidic however it encourages the growth of acid-creating bacteria in your mouth, causing tooth erosion and tooth decay).
Certain medications such as aspirin and antihistamines.
Looking for dental treatment for Bulimia Nervosa, Anorexia Nervosa And Gastric Reflux ?
Call us now at 02 9558 8988 or email us at info@painfreedentistsydney.com.au to organise a consultation today!